Most sore throats heal without complications. But when tonsil inflammation progresses rapidly, recognizing the warning signs can prevent a dangerous situation from becoming life-threatening.
Tonsillitis becomes an emergency when it causes difficulty breathing, severe throat swelling, inability to swallow fluids, a fever above 103°F, signs of dehydration, or symptoms suggesting a peritonsillar abscess. Seek immediate ER care if breathing or swallowing becomes compromised.
This guide covers the red flags that distinguish routine tonsillitis from a medical emergency, what complications can develop, and how emergency rooms treat severe cases.
What Is Tonsillitis?
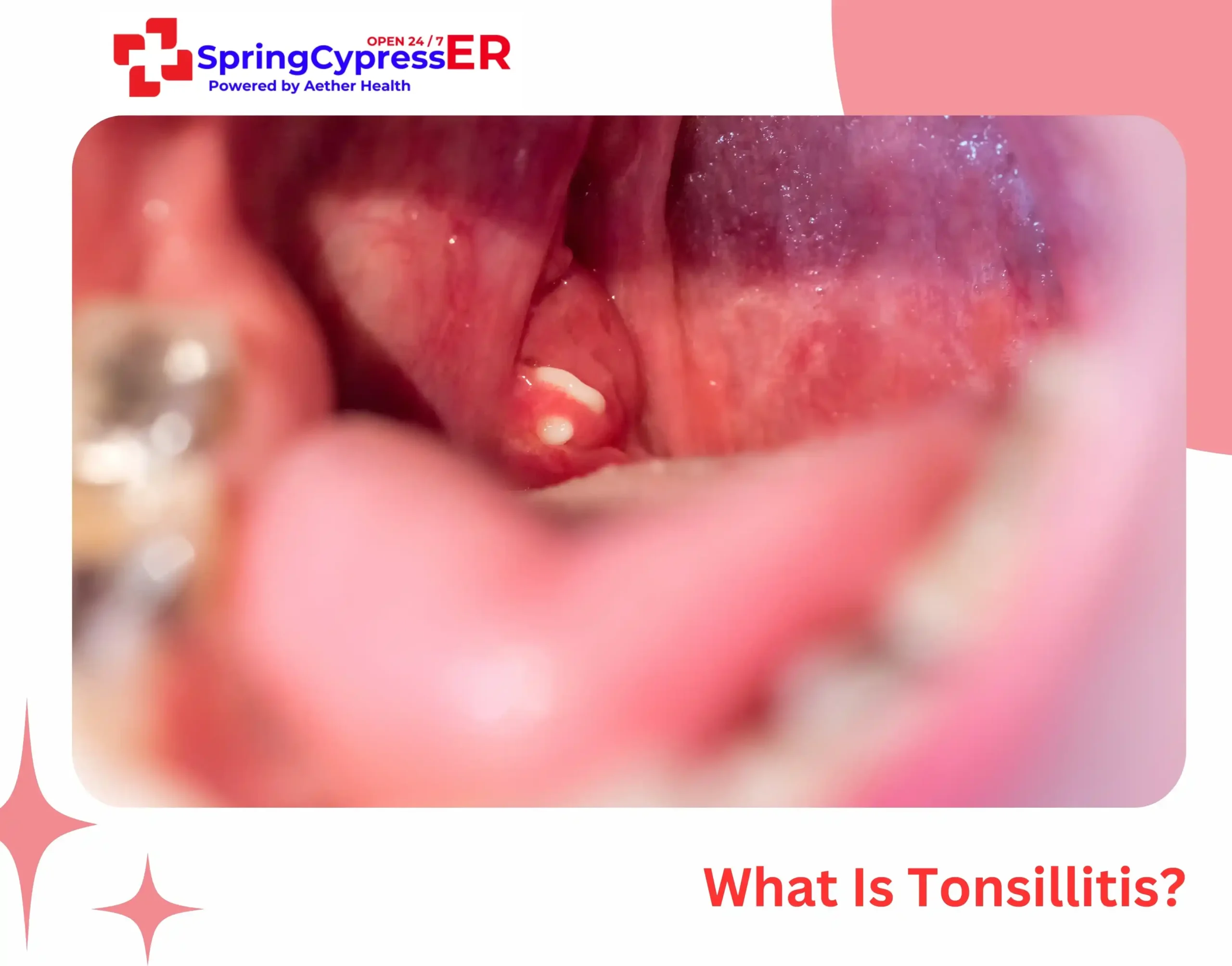
Tonsillitis is inflammation of the tonsils, the two oval-shaped tissue pads located at the back of your throat. These glands serve as your immune system’s first defense against bacteria and viruses entering through the mouth.
When the tonsils become infected, they swell and may develop white or yellow patches. The infection is usually caused by common viruses (like those responsible for colds and flu) or Group A Streptococcus bacteria (the same bacteria responsible for strep throat).
Tonsillitis affects children more frequently because their immune systems are still developing and they have greater exposure to germs at school. Most cases improve with rest, fluids, and medical treatment when needed, but some progress into emergencies requiring rapid evaluation in the ER.
Read More: Tonsillitis vs. Strep Throat
Common Symptoms of Tonsillitis
Recognizing typical tonsillitis symptoms helps you distinguish between a manageable infection and one requiring urgent care. Common tonsillitis symptoms include:
- Sore throat
- Painful swallowing
- Fever
- Red, swollen tonsils
- White or yellow patches
- Bad breath
- Swollen lymph nodes in the neck
- Scratchy or muffled voice
- Ear or jaw pain
- Fatigue
These symptoms alone do not make tonsillitis an emergency. The next section explains when it becomes serious.
When Is Tonsillitis an Emergency? (Detailed Guide)
Tonsillitis becomes a medical emergency when symptoms affect breathing, swallowing, hydration, or when dangerous complications develop. Watch for these red flags:
1. Difficulty Breathing or Noisy Breathing (Stridor)
Severe swelling can partially or completely obstruct the airway, especially in bacterial tonsillitis or abscess formation. Stridor, a high-pitched breathing sound, indicates airway narrowing and requires immediate intervention. Children are more prone to breathing difficulty due to their smaller airways.
2. High Fever Above 103°F (39.4°C)
A very high fever suggests severe bacterial infection that may not respond to oral antibiotics alone. Persistent high fever despite medication warrants emergency evaluation.
3. Inability to Swallow Saliva (Drooling)
Drooling in older children or adults signals that throat swelling has become too severe to manage normal secretions. This classic emergency sign often indicates peritonsillar abscess formation.
4. Dehydration From Inability to Drink
When swallowing becomes too painful, patients stop drinking fluids. Signs of dehydration include dry lips and mouth, decreased urination, dark urine, dizziness, rapid heartbeat, and lethargy.
5. Muffled or “Hot Potato” Voice
A voice that sounds like the person is speaking with a hot object in their mouth often indicates peritonsillar abscess. This dangerous complication can rapidly progress to airway obstruction.
6. Severe Neck Pain or Stiff Neck
Neck stiffness or severe pain may indicate infection spreading to deeper neck spaces (retropharyngeal abscess) or even meningitis. Both require urgent evaluation.
- Unilateral Severe Throat Pain
Pain significantly worse on one side strongly suggests abscess formation. The asymmetry helps distinguish dangerous complications from typical bilateral tonsillitis.
8. Symptoms Worsening After 48–72 Hours of Treatment
If prescribed antibiotics aren’t improving symptoms within 2-3 days, an ER visit is necessary for reassessment or IV treatment.
Also Read: Guide to Respiratory System Emergencies
Complications That Turn Tonsillitis Into an Emergency
Without proper treatment, tonsillitis can progress into dangerous complications requiring emergency intervention.
Peritonsillar Abscess (Quinsy)
The most common serious complication, peritonsillar abscess occurs when infection spreads beyond the tonsil and forms a pus-filled pocket in surrounding tissue. It typically affects one side and causes:
- Severe one-sided throat pain
- Trismus (difficulty opening mouth)
- Muffled voice
- Drooling
- Fever
- Visible bulging near the affected tonsil
- Uvula deviation away from the affected side
Peritonsillar abscess requires emergency drainage and IV antibiotics. Left untreated, it can obstruct the airway or spread infection to the chest.
Airway Obstruction
The most dangerous immediate complication. Severely enlarged tonsils can block airflow, particularly during sleep. Children with naturally smaller airways face greater risk. Warning signs include stridor, retractions (visible pulling of skin between ribs during breathing), and cyanosis (bluish skin color).
Rheumatic Fever
Untreated strep throat can trigger rheumatic fever 2-4 weeks after the initial infection. This inflammatory condition can permanently damage heart valves. Symptoms include joint pain, fever, chest pain, and a distinctive rash. Proper antibiotic treatment prevents this complication.
Post-Streptococcal Glomerulonephritis
Another delayed complication of strep throat, this kidney inflammation causes blood in urine, decreased urination, swelling, and high blood pressure. It typically occurs 1-2 weeks after untreated strep infection.
Spread of Infection
Infection can spread from the tonsils to the neck, chest, or bloodstream:
- Retropharyngeal abscess: Infection in the space behind the throat
- Parapharyngeal abscess: Infection in the deep neck space
- Mediastinitis: Spread to the chest cavity (rare but life-threatening)
- Sepsis: Bacteria entering the bloodstream
Secondary Ear and Sinus Infections
The same bacteria or viruses causing tonsillitis can spread to adjacent structures. Ear infections (otitis media) and sinus infections (sinusitis) frequently accompany or follow tonsillitis, particularly in children.
Types of Tonsillitis
Understanding the different forms of tonsillitis helps explain why some cases become emergencies while others resolve quickly.
Acute Tonsillitis
The most common form, acute tonsillitis develops suddenly and typically lasts 3-10 days. Viral infections cause most acute cases, though bacterial strep throat requires antibiotic treatment. Symptoms include sore throat, fever, and swollen tonsils.
Recurrent Tonsillitis
When acute tonsillitis occurs multiple times per year, it becomes recurrent tonsillitis. Doctors typically define this as seven or more episodes in one year, five episodes per year for two consecutive years, or three episodes per year for three consecutive years.
Chronic Tonsillitis
Chronic tonsillitis involves persistent symptoms lasting longer than two weeks. Patients experience ongoing sore throat, bad breath, and tender cervical lymph nodes. Tonsil stones (tonsilloliths) often accompany this condition.
Bacterial vs. Viral Tonsillitis
Distinguishing between bacterial and viral tonsillitis matters because treatment differs significantly. Viral tonsillitis resolves on its own, while bacterial infections, particularly strep throat, require antibiotics to prevent serious complications like rheumatic fever.
Signs suggesting bacterial tonsillitis:
- Fever above 101°F
- Swollen, tender lymph nodes
- White patches on tonsils
- Absence of cough
- Rapid symptom onset
How the ER Treats Severe Tonsillitis

Emergency rooms provide rapid assessment and treatment for severe tonsillitis and its complications.
✔ Rapid Strep Testing + Throat Cultures
To determine whether the infection is bacterial or viral. A throat culture is more accurate, but results take longer than rapid tests.
✔ Blood tests
Assess infection severity, hydration status, and kidney function.
✔ IV Antibiotics
For severe bacterial tonsillitis or when oral antibiotics fail.
✔ IV Fluids
Restore hydration when swallowing is compromised.
✔ Steroids
To reduce swelling and help breathing.
✔ Pain & Fever Relief
Fast-acting medications for comfort.
✔ CT Scans or Ultrasound
Identify abscess formation or deep neck space infections.
✔ Emergency Drainage
If a peritonsillar abscess is confirmed.
Some patients require observation to monitor breathing, hydration status, and response to treatment before safe discharge.
How to Prevent Severe Tonsillitis

While not all tonsillitis cases are preventable, these measures reduce infection risk and severity:
- Practice good hand hygiene
- Avoid sharing drinks and utensils
- Replace toothbrush after strep diagnosis
- Treat infections early
- Stay hydrated
- Strengthen immunity with sleep & nutrition
Tonsillitis in Children
Children develop tonsillitis more frequently than adults and face higher complication risks. Their smaller airways mean swelling causes proportionally greater obstruction.
When to seek emergency care for a child:
- Breathing difficulty or noisy breathing
- Drooling or inability to swallow
- Refusal to drink fluids
- Signs of dehydration (no wet diapers for 8+ hours, no tears when crying)
- Fever above 103°F
- Excessive sleepiness or difficulty waking
- Neck stiffness
- Severe throat pain preventing eating or drinking
Young children cannot always articulate their symptoms. Watch for behavioral changes like unusual fussiness, refusal to eat, or pulling at their ears and throat.
FAQs
1. Can tonsillitis go away on its own?
Yes, viral tonsillitis typically resolves on its own within 7-10 days with rest, fluids, and over-the-counter pain relief. However, bacterial tonsillitis caused by strep throat requires antibiotic treatment to prevent complications.
2. Is strep throat the same as tonsillitis?
No, strep throat is one specific cause of tonsillitis, not a separate condition. Tonsillitis refers to inflamed tonsils regardless of cause. Strep throat means Group A Streptococcus bacteria caused the inflammation. Many viruses also cause tonsillitis.
3. How long does tonsillitis last?
Tonsillitis typically lasts 7-10 days. Viral cases often improve within a week while bacterial tonsillitis symptoms usually begin improving within 2-3 days of starting antibiotics, though the full course must be completed. Symptoms persisting beyond 10 days warrant medical attention.
4. Can tonsillitis turn into pneumonia?
Tonsillitis does not directly become pneumonia. However, untreated strep can cause serious complications.
5. Does tonsillitis always need antibiotics?
No, only bacterial tonsillitis requires antibiotics. Since viruses cause most tonsillitis cases, antibiotics would be ineffective and contribute to antibiotic resistance. Doctors use rapid strep tests or throat cultures to determine whether bacteria are responsible.
6. What does a peritonsillar abscess feel like?
A peritonsillar abscess causes severe one-sided throat pain that worsens rapidly. Patients often describe difficulty opening their mouth fully, a muffled voice, drooling, and pain radiating to the ear on the affected side. High fever accompanies these symptoms.
7. Can tonsillitis cause ear pain?
Yes, tonsillitis commonly causes ear pain through referred pain pathways. The throat and ears share nerve connections, so inflammation in the throat can create sensations felt in the ear. Additionally, infection can spread from the throat to the middle ear, causing actual ear infection (otitis media), especially in children.
Need Emergency Care for Severe Tonsillitis? Walk In 24/7
If you or your child experiences breathing difficulty, drooling, high fever, severe swelling, or worsening throat pain, visit Aether Health – Spring Cypress ER immediately. Our board-certified emergency physicians provide rapid evaluation and treatment 24/7, including IV antibiotics, hydration therapy, and abscess drainage when needed.
[Call Now] or [Get Directions]